En este laboratorio se trabaja en el entorno de las enfermedades infecciosas, realizando deteccción y caracterización de agentes infecciosos (virus o bacteria), asi como su relación con el huésped.

En este laboratorio se trabaja en el entorno de las enfermedades infecciosas, realizando deteccción y caracterización de agentes infecciosos (virus o bacteria), asi como su relación con el huésped.
Jefe del laboratorio
Maria Jesus Pons Casellas
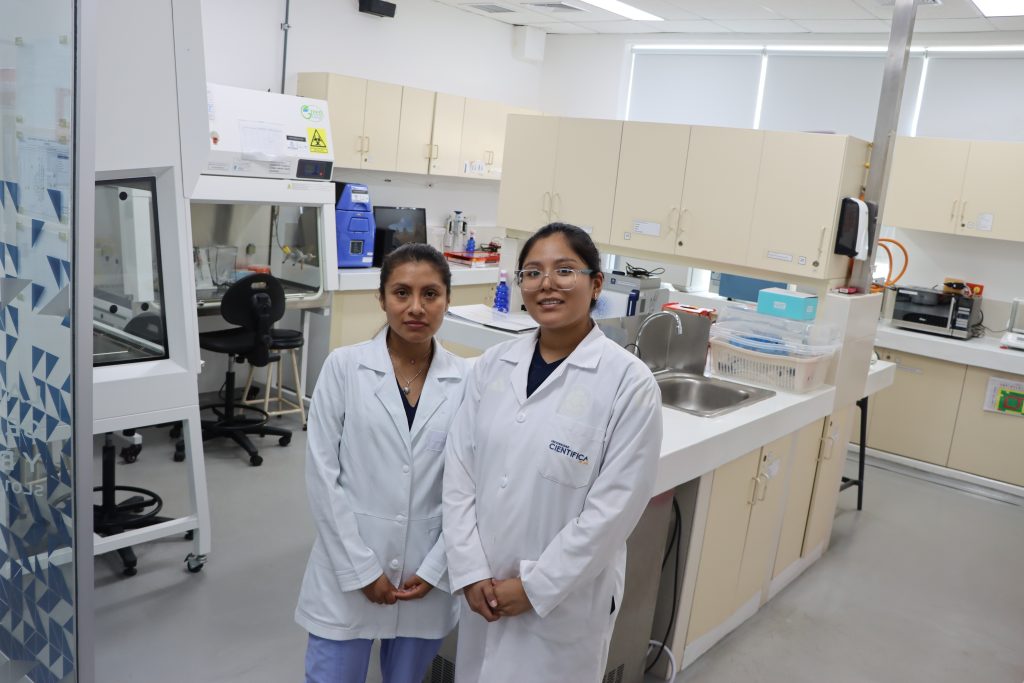
Kathya Cecilia Espinoza Ramirez – Investigadora Asistente
Gabriela Jareth Silva Zamora – Auxiliar Técnico de Laboratorio
Cambio climático y agua- Ambiente y biodiversidad
Inmunidad, cáncer y enfermedades crónicas -Salud y bienestar
Microbiología, infecciosas y one health- Salud y bienestar
Producción animal sostenible y seguridad alimentaria – Desarrollo sostenible
Centrifuga Refrigerada
Cubeta de Electroforesis con fuente de poder
Cabina de Bioseguridad Clase II
Termociclador
Termociclador PCR Tiempo Real
Microcentrifuga
Termobloque Digital
Incubadora CO2
Turbidimetro
Balanza Analítica
Captador de imagenes (filtro azul y BrEt)
Detección de agentes infecciosso (PCR convencional o qPCR).
Caracterización del agente (factores virulencia, factores de resistencia y clonalidad).
Relación de agentes infecciosos y su relación con los huespedes (medición biomarcadores- ELISA y/o MAGPIX)
Gemma Moncunill – España
Clauda Paradela Gomes – Portugal
Gabriela Soza – INMP-Perú
Instituto de Salud Global de Barcelona – Laboratorio de Ecología Microbiana
Facultad de Ciencias Biológicas de Universidad Nacional Mayor de San Marcos, Lima, Perú
Instituto Nacional Materno Perinatal, Lima, Perú.
Carrion's disease is a neglected endemic disease found in remote Andean areas. As an overlooked disease, knowledge of innate immune responses to Bartonella bacilliformis, the etiological agent, is scarce. This study aimed to evaluate the cytokine response to B. bacilliformis using in vitro human peripheral blood mononuclear cells (PBMCs) stimulations. PBMCs from naive adults were isolated by gradient centrifugation and cocultured with heat-inactivated (HI) B. bacilliformis at different incubation times (3, 6, 12, 24, and 36 h). Cytokines, chemokines, and growth factors were determined in culture supernatants by multiplex fluorescent bead-based quantitative suspension array technology. During the first 36 h, a proinflammatory response was observed, including tumor necrosis factor-α, interleukin (IL)-1α, IL-1β, interferon-α2, and IL-6, followed by an anti-inflammatory response mainly related to IL-1RA. Moreover, high expression levels of chemokines IL-8, monocyte chemoattractant protein-1α, and macrophage inflammatory protein (MIP)-1β were detected from 3 h poststimulation and MIP-1α was detected at 24 h. Some growth factors, mainly granulocyte macrophage colony-stimulating factor and granulocyte colony-stimulating factor, and in minor concentrations vascular endothelial growth factor, epidermal growth factor, and eotaxin, were also detected. Innate response to HI B. bacilliformis stimulation consists of a rapid and strong proinflammatory response characterized by a wide range of cytokines and chemokines followed by an anti-inflammatory response and increased specific growth factors.
Innate immune responses through the production of type I interferon-α (anti-IFN-α) play an essential role in the defense against viruses. The autoantibodies (auto-Abs) anti-IFN-α are implicated in COVID-19 pathogenesis with higher levels among patients with worse prognoses. The study aimed to assess the levels of anti-IFN-α auto-Abs in Peruvian patients with severe/critical hospitalized COVID-19 compared to asymptomatic/mild COVID-19 outpatients and healthy controls. We analyzed 101 serum samples, including 56 (55.5%) severe/critical, 13 (12.3%) asymptomatic/mild COVID-19 patients, and 32 (32.2%) healthy controls, which we tested using a commercial ELISA anti-IFN-α-auto-Abs kit. We observed seropositivity of 48.2% (26/54) to anti-IFN-α auto-Abs among the severe/critical COVID-19 group, but 0% (0/13) and 3.1% (1/32) among the asymptomatic/mild COVID-19 and healthy groups (P = 0.021), respectively. Furthermore, we observed a significant association between the log10 of anti-IFN-α auto-Abs and the COVID-19 status, with the log10 of anti-IFN-α auto-Abs levels being significantly higher among the severe/critical COVID-19 group compared to the healthy controls (β = 1.20; confidence interval [95% CI]: 0.72–1.67; P < 0.001). Such association remains significant either when adjusted by age and gender (adjusted β = 1.16; 95% CI: 0.62–1.70; P < 0.001) and when adjusted by the subjects age, gender, and obesity (adjusted β = 1.16; 95% CI: 0.62–1.70; P < 0.001). Despite not measuring neutralizing activity, this study highlights the high frequency of these auto-Abs in the Peruvian population with a worse prognosis of COVID-19.

This study aimed to analyze Escherichia coli from marketed meat samples in Peru. Sixty-six E. coli isolates were recovered from 21 meat samples (14 chicken, 7 beef), and antimicrobial resistance levels and the presence of mechanisms of antibiotic resistance, as well as clonal relationships and phylogeny of colistin-resistant isolates, were established. High levels of antimicrobial resistance were detected, with 93.9% of isolates being multi-drug resistant (MDR) and 76.2% of samples possessing colistin-resistant E. coli; of these, 6 samples from 6 chicken samples presenting mcr-1-producer E. coli. Colistin-resistant isolates were classified into 22 clonal groups, while phylogroup A (15 isolates) was the most common. Extended-spectrum β-lactamase- and pAmpC-producing E. coli were found in 18 and 8 samples respectively, with blaCTX-M-55 (28 isolates; 16 samples) and blaCIT (8 isolates; 7 samples) being the most common of each type. Additionally, blaCTX-M-15, blaCTX-M-65, blaSHV-27, blaOXA-5/10-like, blaDHA, blaEBC and narrow-spectrum blaTEM were detected. In addition, 5 blaCTX-M remained unidentified, and no sought ESBL-encoding gene was detected in other 6 ESBL-producer isolates. The tetA, tetE and tetX genes were found in tigecycline-resistant isolates. This study highlights the presence of MDR E. coli in Peruvian food-chain. The high relevance of CTX-M-55, the dissemination through the food-chain of pAmpC, as well as the high frequency of unrelated colistin-resistant isolates is reported.

Cytokines, chemokines and growth factors present different expression profiles related to the prognosis of COVID-19. We analyzed clinical parameters and assessed the expression of these biomarkers in patients with different disease severity in a hospitalized Peruvian cohort to determine those associated with worse prognosis. We measured anti-spike IgG antibodies by ELISA and 30 cytokines by quantitative suspension array technology in 123 sera samples. We analyzed differences between patients with moderate, severe and fatal COVID-19 by logistic regression at baseline and in longitudinal samples. Significant differences were found among the clinical parameters: hemoglobin, neutrophils, lymphocytes and C-reactive protein (CRP), creatinine and D-dimer levels. Higher anti-spike IgG antibody concentrations were associated to fatal patient outcomes. At hospitalization, IL-10, IL-6, MIP-1α, GM-CSF, MCP-1, IL-15, IL-5, IL1RA, TNFα and IL-8 levels were already increased in fatal patients´ group. Meanwhile, multivariable analysis revealed that increased GM-CSF, MCP-1, IL-15, and IL-8 values were associated with fatal outcomes. Moreover, longitudinal analysis identified IL-6 and MCP-1 as the main risk factors related to mortality in hospitalized COVID-19 patients. In this Peruvian cohort we identified and validated biomarkers related to COVID-19 outcomes. Further studies are needed to identify novel criteria for stratification of SARS-CoV-2 infected patients at hospital entry.